Asthma
Residents of the St. Louis region have long experienced high asthma rates.¹ Within the region, the asthma burden is felt most heavily in the City of St. Louis.² And within the City, the burden falls most heavily on black residents.
Several of the factors explored later in this report—including mold and air pollution—together with poor quality housing and limited access to preventive health care contribute to the significant racial disparity for asthma.³ As Figure 2.1 shows, black St. Louisans made 8.5 times more visits to the emergency room (per 1,000 residents) for asthma than did white St. Louisans between 2010 and 2015.⁴ The gap is even wider among the City’s children. Black children in St. Louis made 10.8 times more emergency room visits for asthma (42.44 visits per 1,000 children) than did white children (3.93 visits per 1,000 children) in 2015.⁵ The City’s 2018 Equity Indicators Baseline Report gave St. Louis the lowest possible score for racial inequity (1 out of 100) regarding childhood asthma.⁶
FIGURE 2.1. NUMBER OF EMERGENCY ROOM VISITS (PER 1,000 RESIDENTS) DUE TO ASTHMA IN ST. LOUIS BY RACE, 2010-2015⁷
The zip code comparisons in Figures 2.2 and 2.3 further demonstrate the racial disparity for asthma in St. Louis. As shown in Figure 2.2, the zip codes with the highest number of emergency room visits due to asthma in 2015—63106 and 63107 in North City and 63118 in South City—are majority-black. Furthermore, all zip codes in North City, which are all majority-black, were in the two highest tiers for asthma emergency room visit rates in 2015. In contrast, the zip codes with the lowest asthma emergency room visit rates in 2015 are either majority-white (63109 and 63139) or have no racial majority (63108).⁸
FIGURE 2.2. NUMBER OF EMERGENCY ROOM VISITS (PER 1,000 RESIDENTS) DUE TO ASTHMA BY ZIP CODE, 2015⁹
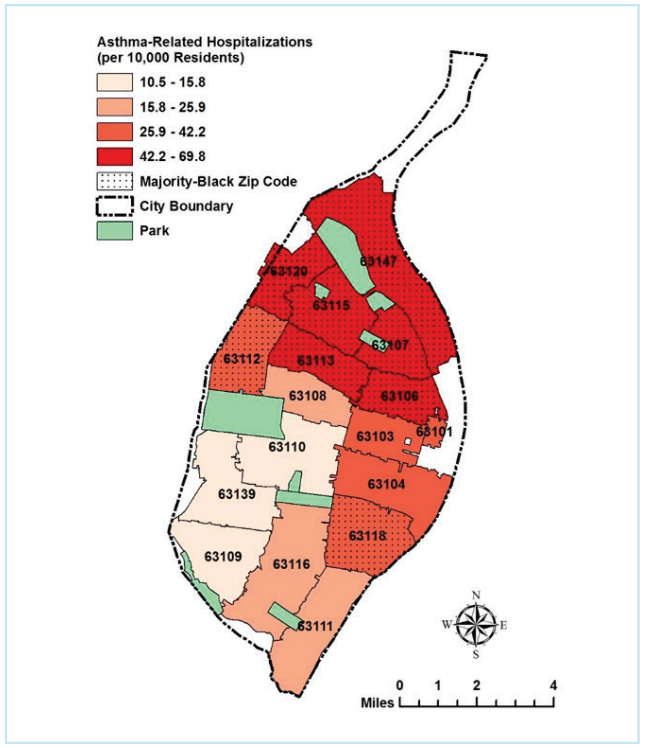
Similarly, as shown in Figure 2.3, asthma hospitalization rates were highest in six majority-black zip codes in North City and lowest in three majority-white zip codes in South City between 2012 and 2014.
FIGURE 2.3. NUMBER OF HOSPITALIZATIONS (PER 10,000 RESIDENTS) DUE TO ASTHMA BY ZIP CODE, 2012-2014¹⁰
These racial disparities in asthma within the City’s population are further magnified when comparing St. Louis with surrounding counties and the rest of the state. As shown in Figure 2.4, asthma-related emergency room visit rates were significantly higher in 2015 for City residents than for residents of St. Louis County, St. Charles County, and the state of Missouri. However, this burden is borne disproportionately by the City’s black residents, while the City’s white residents actually fare better than whites statewide. The asthma-related emergency room visit rate for white City residents (2.9 visits per 1,000 residents) is well below the statewide average (5.3 visits per 1,000 residents).¹¹ In sharp contrast, the rate for black City residents (24.7 visits per 1,000 residents) is about 4.6 times higher than the statewide average.¹²
The Impacts of Asthma
Asthma is a lung disease which makes it harder to breathe due to swollen or enflamed airways.¹⁴ While asthma has no cure and can be life-threatening, with good medical care it can be managed.¹⁵ Unfortunately, lack of access to adequate medical care also disproportionately affects minority communities.¹⁶ Common asthma triggers include air pollution, stress, illness, smoking, and exposure to allergens such as mold, pollen, dust, dust mites, and pets.¹⁷ At least two of those triggers—air pollution and mold—also disproportionately affect black St. Louisans.
FIGURE 2.4. COMPARISON OF ASTHMA-RELATED EMERGENCY ROOM VISIT RATES FOR ST. LOUIS CITY, ST. LOUIS AND ST. CHARLES COUNTIES, AND MISSOURI, 2015¹³
M.J.’S Family Struggles with Asthma
M.J. is a mother to a 22-year-old son who has had asthma for many years. When they moved into their current apartment in Dutchtown, M.J.’s son had a flare up right away and went to the hospital. He was treated, stayed overnight, and then was better. Afterwards, his 6-year-old step-daughter, who was then staying with M.J. and her son, had an asthma attack and had to go to the emergency room. The step-daughter never had asthma before this.
M.J.’s son switched bedrooms with his step-daughter, and he had an asthma attack and had to go to the emergency room. They suspected that the room might be triggering the asthma attacks, and found what looked like mold in the corner. M.J.’s son now has to use his inhaler again, and his step-daughter is using both an inhaler and a breathing machine. M.J. has told her landlord about the mold, but he hasn’t yet responded. The last time she found mold in another room, the landlord told her he would give her some paint to cover it up, but that didn’t solve the mold problem.
M.J.’s family’s health is put at risk by unsafe housing conditions that are difficult if not impossible to detect before signing a lease.
References
¹ East-West Gateway, Where We Stand, 4th Edition, Update 1, Asthma and Allergy Risk Factors in the St. Louis Region (Apr. 2004), p. 1, available at https://www.ewgateway.org/wp-content/ uploads/2017/08/WWS4EdNo1.pdf (St. Louis region ranked number one among peer metropolitan regions for asthma risks); OzarksFirst.com, St. Louis Named Top Asthma Capital for 2009 (Jan 28, 2009), available at https://www.ozarksfirst.com/news/health-and-medical/st-louis-named-top-asthma-capital-for-2009/74979576; East-West Gateway, Where We Stand, 6th Edition, Update 3, Where We Stand Update: Twenty Years Later (Jan. 2013), pp. 16-17, available at https://www.ewgateway.org/wp-content/uploads/2017/08/WWS6EdNo3.pdf (St. Louis region number one among peer regions for asthma risks in 2010; although 30 of the 35 regions studied reduced their asthma risks from 2006 to 2010, “St. Louis was one of the five regions that saw an increase in asthma risk.”).
² See infra, Figure 2.3 and p.8
³ City of St. Louis Department of Health, Asthma Data Brief (Mar. 20, 2018), p. 1, available at https://www.stlouis-mo.gov/government/departments/health/documents/upload/Asthma-Data-Brief03-20-2018-2-hb.pdf (“2018 Asthma Data Brief”); East-West Gateway, Where We Stand, 4th Edition, Update 1, Asthma and Allergy Risk Factors in the St. Louis Region (Apr. 2004), p. 1, available at https://www.ewgateway.org/wp-content/uploads/2017/08/WWS4EdNo1.pdf (St. Louis region ranked number one among peer metropolitan regions for asthma risks).
⁴ 2018 Asthma Data Brief, p. 2. The data reflect total emergency room visits for asthma, not visits by different individuals. The emergency room disparities may also reflect disparities in access to preventive health care and lower-cost treatments.
⁵ Equity Indicators Report, p. 36. The data are based on total emergency room visits during 2015, not visits by different children. “Children” includes those age 19 and younger
⁶ Id.
⁷ 2018 Asthma Data Brief, p. 2.
⁸ See Equity Indicators Report, p. 261.
⁹ Prepared by the Interdisciplinary Environmental Clinic. Data Sources: 2018 Asthma Data Brief, p. 2; Equity Indicators Report, p. 261.
¹⁰ Prepared by the Interdisciplinary Environmental Clinic. Data Sources: Think Health St. Louis, Age-Adjusted Hospitalization Rate Due to Asthma, 2012-2014 Measurement Period, available at http://www.thinkhealthstl.org/?module=indicators&controller=index&action=view&localeFilterId=1649&comparisonId=&indicatorId=14&localeTypeId=3; Equity Indicators Report, p. 261.
¹¹ Compare Figures 2.1 and 2.4.
¹² Id.
¹³ 2018 Asthma Data Brief, p. 1.
¹⁴ American Lung Association, What is Asthma, available at https://www.lung.org/lung-health-and-diseases/lung-disease-lookup/asthma/learn-about-asthma/what-is-asthma.html.
¹⁵ Id.
¹⁶ The Asthma and Allergy Foundation of America and The National Pharmaceutical Council, Ethnic Disparities in the Burden and Treatment of Asthma (Jan. 2005), p. iii, available at https://www.aafa.org/media/1633/ethnic-disparities-burden-treatment-asthma-report.pdf.
¹⁷ Palo Alto Medical Foundation, Common Asthma Triggers, available at http://www.pamf.org/asthma/overview/triggers.html#Other%20Triggers; see also CDC, Common Asthma Triggers, available at https://www.cdc.gov/asthma/triggers.html.